Comprehensive Guide to Pelvic Floor Dysfunction: Causes, Symptoms, Diagnosis, and Treatment
Pelvic floor dysfunction (PFD) is a common condition that can significantly impact an individual’s quality of life. This comprehensive guide explores the underlying causes, key symptoms, diagnostic methods, and available treatment options for managing pelvic floor dysfunction. By understanding the intricacies of PFD and the approaches to addressing it, individuals can take proactive steps toward restoring pelvic health and improving overall well-being. For further insights, you can explore our detailed blog on Pelvic Floor Therapy in Dubai at Feto Maternal & GenetYX Center.
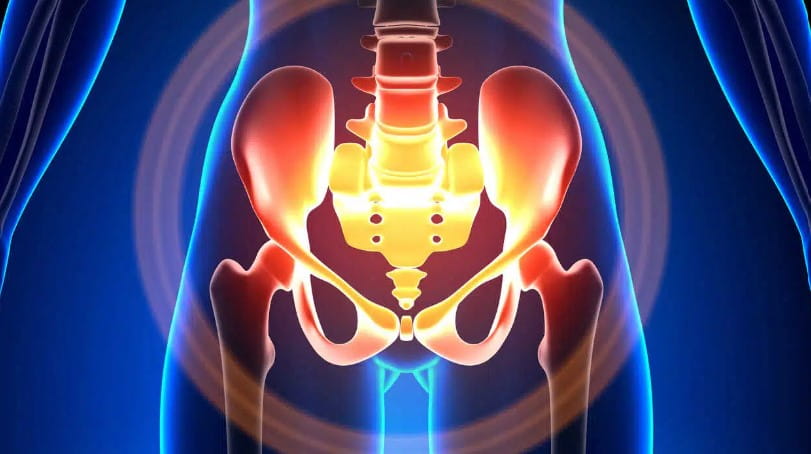
Detailed Anatomy of the Pelvic Floor
Understanding the anatomy of the pelvic floor is crucial for diagnosing and managing pelvic floor dysfunction.
Key Components of the Pelvic Floor:
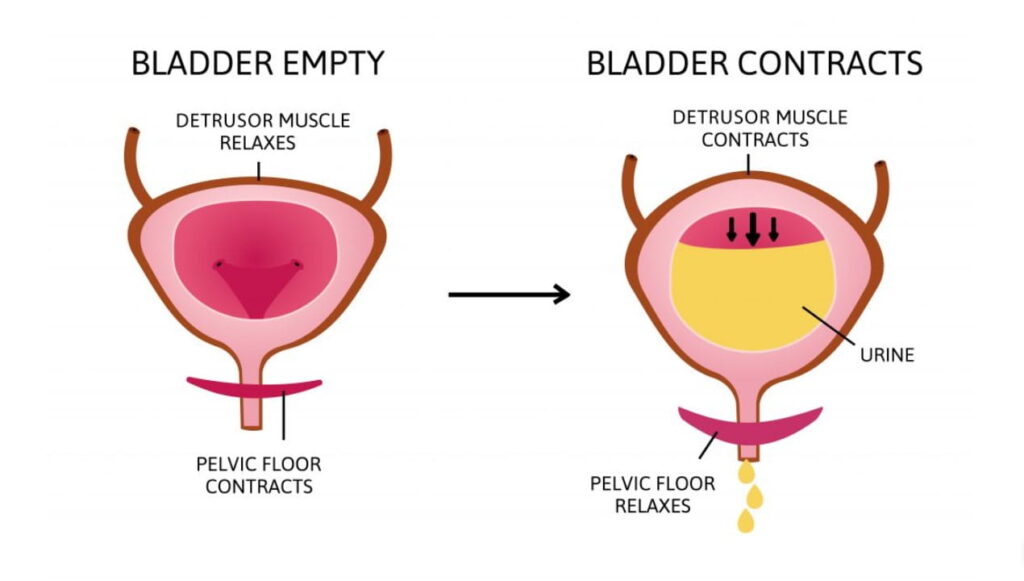
- Pelvic Muscles: These muscles form a supportive sling at the base of the pelvis, essential for controlling bladder, bowel, and sexual functions.
- Connective Tissues: Ligaments and fascia provide additional support and stability to the pelvic organs.
- Supported Organs: Includes the bladder, rectum, uterus (in women), and prostate (in men).
Causes of Pelvic Floor Dysfunction
Pelvic floor dysfunction can arise from various factors, including:
- Childbirth: Vaginal delivery can stretch or tear pelvic floor muscles and tissues, leading to dysfunction.
- Chronic Constipation: Frequent straining during bowel movements can weaken the pelvic muscles.
- Aging: Natural aging can lead to decreased muscle tone and strength, contributing to dysfunction.
- Surgical Procedures: Surgeries involving the pelvic area can impact pelvic floor function.
Symptoms and Conditions Linked to Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction can vary but often include:
- Urinary Incontinence: Involuntary leakage of urine, often triggered by physical activities or sneezing.
- Pelvic Pain: Persistent or intermittent pain in the pelvic region.
- Pelvic Pressure: A feeling of heaviness or pressure in the pelvic area.
- Difficulty with Bowel Movements: Issues such as constipation or incomplete evacuation.
Diagnostic Approaches
Effective diagnosis is essential for managing pelvic floor dysfunction. Common diagnostic methods include:
- Physical Exams: Assess muscle strength and identify abnormalities through a thorough physical examination.
- Imaging Techniques: Use ultrasound or MRI to obtain detailed images of pelvic floor structures.
Non-Surgical Treatment Options
Several non-surgical treatments can help manage pelvic floor dysfunction:
- Lifestyle Changes: Incorporate regular exercise, maintain a healthy weight, and manage stress effectively.
- Self-Care: Engage in pelvic floor exercises, such as Kegels, to strengthen the muscles.
- Biofeedback: Utilize sensors to provide real-time feedback on muscle activity, aiding in control and strengthening.
Long-Term Outcomes of Pelvic Floor Therapy
Pelvic floor therapy can lead to significant improvements. Consider the following patient success stories:
- Patient Success Story: “After committing to pelvic floor therapy and incorporating recommended exercises, my urinary incontinence and pelvic pain have greatly reduced. My quality of life has improved significantly. – Kristy”
Risks and Limitations of Pelvic Floor Therapy
Potential risks and limitations include:
- Individual Variability: Treatment effectiveness may vary based on individual conditions.
- Time Commitment: Requires consistent effort and follow-up appointments to see results.
- Potential Discomfort: Some initial discomfort or soreness may occur during therapy.
Treatment Options Beyond Therapy
Other treatment options for pelvic floor dysfunction may include:
- Medication: Used for managing symptoms such as urinary incontinence or pelvic pain.
- Surgical Options: In severe cases, surgical interventions may be necessary.
- Lifestyle Adjustments: Ongoing changes to diet and exercise can support pelvic health.
Pelvic floor dysfunction can significantly impact daily life, but with proper diagnosis and treatment, many individuals experience relief and regain control over their pelvic health. Whether through non-surgical therapies, lifestyle changes, or medical interventions, it’s important to understand that help is available. By addressing the symptoms early and working with healthcare professionals, you can improve your quality of life. If you suspect you may be dealing with pelvic floor dysfunction, don’t hesitate to seek professional advice and explore the available treatment options. Your path to recovery may just be a step away.

